By Lesiba Machaka
In the wide-open villages of Limpopo-where gravel roads breathe dust and rumours often outrun clinic vans, access to clear, reliable health information remains a privilege rather than a guarantee. Before dawn, elderly women queue outside ageing clinics, holding onto hope that today someone will explain what yesterday did not. Inside, overstretched nurses work through staff shortages, limited resources, and systems running on fumes.
Across government, academia, labour unions and civil society, one reality is becoming increasingly difficult to ignore: rural communities are still fighting for clarity, for trust, and for health education that reaches them in ways they can understand.
Department of Health says it continues to push health information into remote areas despite mounting constraints. Spokesperson Foster Mohale explains that the department relies on community healthcare workers, community radio stations, vernacular media interviews and periodic media training to disseminate verified health messages.
“The Department uses community media and community healthcare workers to share health information. We are not silent,” Mohale says. “These platforms help ensure that crucial health information reaches the public, including people in rural communities.”
He adds that community newspapers remain a vital link between the health system and the public. According to Mohale, publications help ensure that health messages reach communities that may otherwise be excluded from mainstream communication channels.
On the ground, however, many rural residents continue to feel disconnected from the health system, particularly when it comes to consistent information-sharing, outreach and patient education.
For Professor Tivani Mashamba-Thompson, Deputy Dean of Research and Postgraduate Studies in the Faculty of Health Sciences at the University of Pretoria, the crisis is not only about limited resources but also about how information is communicated. Raised in a rural Limpopo community herself, she has witnessed first-hand how misinformation thrives where accurate information is absent.
“Limited access to accurate health information directly impacts people’s well-being,” she explains. “It leads to delayed healthcare-seeking, stigma, and reliance on informal sources that are often unreliable.”
She points to the COVID-19 pandemic as a clear example of how fragile trust in the health system can be. During that period, rumours, fake cures and conspiracy theories spread rapidly in many communities, often outpacing verified scientific information.
Language, she argues, remains one of the most persistent barriers. Health messages delivered in technical English often fail to resonate in rural settings where many residents speak indigenous languages and may have limited formal education.
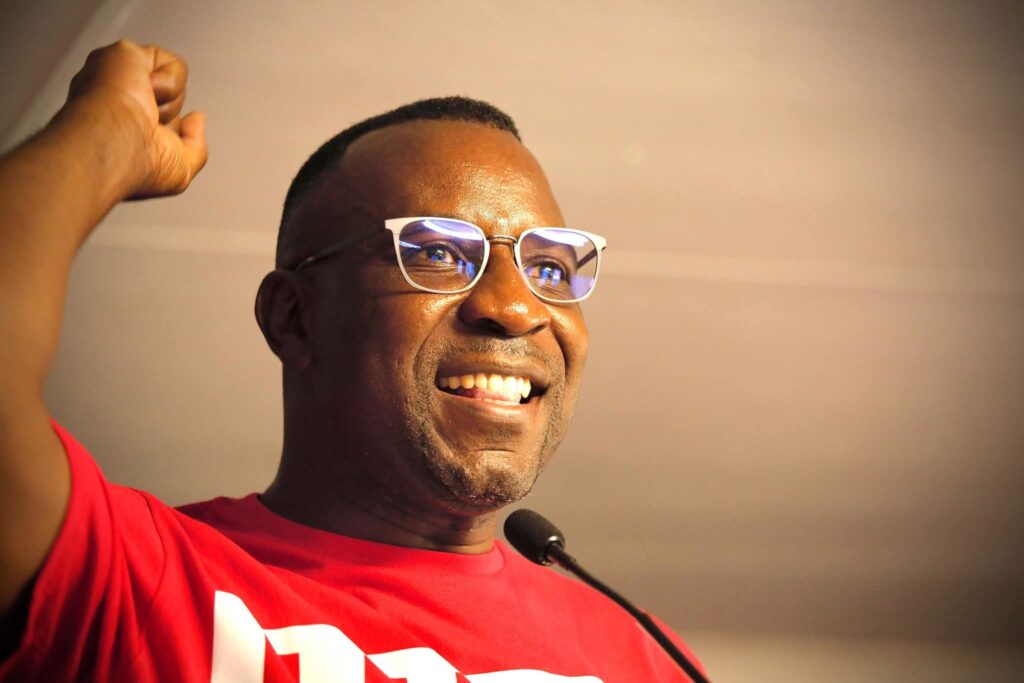
From a labour perspective, National Education Health and Allied Workers’ Union (Nehawu) Limpopo provincial secretary Moses Maubane argues that the province’s health system remains overly focused on treating illness rather than preventing it. He believes this imbalance has left rural communities particularly vulnerable.
“We must invest in preventative health. The curative approach dominates, and it is failing rural people,” says Maubane, pointing to a system that intervenes only once communities are already sick.

In practical terms, preventative healthcare in rural Limpopo could mean regular health talks at clinics before consultations begin, where nurses or trained community health workers explain TB symptoms, HIV treatment adherence, mental health warning signs, and chronic illness management in local languages that they (patients) understand. It could include mobile outreach teams visiting villages to offer basic screening for TB, HIV, diabetes and hypertension before complications arise.
Schools, churches and community halls could serve as spaces for youth-focused health education, helping young people understand sexual health, substance abuse risks and mental well-being early, rather than encountering the health system at a later stage.
Such interventions are widely regarded as cost-effective and life-saving. Early screening reduces the need for hospitalization, consistent health education improves treatment adherence, and trusted local communication helps dispel myths before they harden into stigma. For rural communities, prevention is not an abstract policy idea – it is often the difference between managing illness early or arriving at clinics when options are already limited. Civil society watchdog Treatment Action Campaign (TAC) offers an unfiltered snapshot, drawn straight from clinic benches where truth and myth wrestle in real time.
TAC reports that many rural communities still lack basic, clear information about HIV, TB, diabetes, mental health and treatment adherence.
“Daily health talks – once the heartbeat of patient education have collapsed due to staff shortages,” says Daniel Mathebula, TAC Limpopo Provincial Coordinator.
“Mental health is ignored, even among people living with HIV.”
Inside clinics, posters on TB and HIV have quietly disappeared – some removed because they “damage walls.”
“Venda communities receive English pamphlets. It must change,” Mathebula says.
“Giyani needs Xitsonga. Thohoyandou needs Tshivenda. Capricorn needs Sepedi. People deserve information they can understand.”
From government corridors to village kraals, one truth rings clear: Limpopo’s rural health system stands at a crossroads between science and myth, effort and collapse, information and deadly silence. In the province’s most remote corners, a single clear message delivered consistently, credibly and in the right language can mean the difference between fear and understanding, between delayed treatment and early care, and ultimately between stigma and survival.
















